Exam Details
Exam Code
:USMLE-STEP-2Exam Name
:United States Medical Licensing Step 2Certification
:USMLE CertificationsVendor
:USMLETotal Questions
:738 Q&AsLast Updated
:Jul 30, 2025
USMLE USMLE Certifications USMLE-STEP-2 Questions & Answers
-
Question 711:
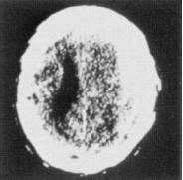
A63-year-old man complains of sudden onset of right-sided headache while at work. He rapidly becomes confused and lethargic. On examination, he is hemiparetic and has bilateral Babinski signs. ACT scan of the head is shown in the figure. What is the patient most likely to have?

A. an arteriovenous malformation
B. a carotid occlusion
C. hypertension
D. an underlying malignancy
E. abnormal clotting studies
-
Question 712:
A 73-year-old man has been experiencing increasing drowsiness and incoherence. He has a history of arrhythmias and has fallen twice in the past 2 weeks. There are no focal deficits on neurologic examination. Acontrast CT scan of the head is shown in the figure below. Which of the following is the treatment of choice?
A. parenteral antibiotics
B. antifungal therapy
C. neurosurgical evacuation of the clot
D. observation and a repeat CT scan in 1 month
E. fibrinolytic therapy
-
Question 713:
A 70-year-old man presents with shuffling gait, tremor, masked facies, and rigidity which have progressed over the last 9 months. Parkinson's disease is diagnosed. Which of the following is not true about Parkinson's disease?
A. Over 1 million people in North America have Parkinson's disease.
B. Mortality is higher in patients with Parkinson's disease when compared to age-matched controls.
C. The classic triad of major signs of Parkinson's disease is memory loss, rigidity, and akinesia.
D. The tremor in Parkinson's disease is typically an intention tremor.
E. Over 90% of patients with Parkinson's disease have a good initial response tolevodopa.
-
Question 714:
A 70-year-old man presents with shuffling gait, tremor, masked facies, and rigidity which have progressed over the last 9 months. Parkinson's disease is diagnosed. In this patient, which neurotransmitter deficiency primarily is responsible for his symptoms?
A. acetylcholine
B. epinephrine
C. norepinephrine
D. dopamine
E. cortisol
-
Question 715:
Which of the following is a useful clue to the diagnosis of Legionella pneumonia?
A. diarrhea
B. rash
C. pedal edema
D. elevated serum glucose
E. photophobia
-
Question 716:
A60-year-old previously healthy man presents with massive rectal bleeding. Which of the following is the most likely diagnosis?
A. diverticulosis of the colon
B. ulcerative colitis
C. external hemorrhoid
D. ischemic colitis
E. carcinoma of the colon
-
Question 717:
A 24-year-old man runs a marathon on an unusually hot and muggy day. Several hours later he becomes ill with fever, weakness, and painful swollen legs and passes dark brown urine. Which of the following is a common finding with this disorder?
A. Urine orthotoluidine (Hematest) reaction will be negative.
B. Serum will be pink.
C. Serum creatine phosphokinase levels will be elevated.
D. Serum haptoglobin levels will be elevated.
E. Serum potassium levels will be lowered.
-
Question 718:
A32-year-old woman is referred to you by her dermatologist for further evaluation. She developed these changes gradually in the last year. Her hands are seen in Figure. What other associated disease is most likely?

A. acquired immune deficiency syndrome (AIDS)
B. Addison's disease
C. lymphoma
D. primary biliary cirrhosis
E. Hashimoto's thyroiditis
-
Question 719:
A59-year-old woman who lives independently and had been healthy, presents to the emergency department with cough and fever. She related she was well until 2 days before when she noted onset of fever, chills, and cough productive of yellow sputum. On examination, you note a tired appearing woman with BP of 160/90, pulse of 105, and respiratory rate of 32. You start her on ceftriaxone and azithromycin and admit her to the hospital. Which of the following factors is a poor prognostic sign in community acquired pneumonia?
A. age less than 60
B. systolic BP = 160 mmHg
C. leukocytosis = 15,000
D. respiratory rate = 32
E. mycoplasma pneumonia infected
-
Question 720:
A 54-year-old man presents to the emergency department complaining of epigastric discomfort, which began while he was walking his dog after dinner about one-half hour earlier. He has not received medical care for several years. On examination, he is moderately obese and in obvious discomfort and seems restless. His BP is 160/98 mmHg, and his examination is otherwise unremarkable. His ECG is seen in Figure below:

Which of the following is the most appropriate next step in management?
A. trial of antacid immediately
B. reassurance and arrange outpatient follow-up
C. arrange for cardiac intensive care bed
D. begin thrombolytic therapy in the emergency department
E. arrange for urgent echocardiogram
Tips on How to Prepare for the Exams
Nowadays, the certification exams become more and more important and required by more and more enterprises when applying for a job. But how to prepare for the exam effectively? How to prepare for the exam in a short time with less efforts? How to get a ideal result and how to find the most reliable resources? Here on Vcedump.com, you will find all the answers. Vcedump.com provide not only USMLE exam questions, answers and explanations but also complete assistance on your exam preparation and certification application. If you are confused on your USMLE-STEP-2 exam preparations and USMLE certification application, do not hesitate to visit our Vcedump.com to find your solutions here.